Why are Slovenians unable to get information about the quality of surgeons who operate on them
The quality of work performed by individual doctors in Slovenia is not being systematically supervised by health officials. This is one of the reasons for much of the recent medical scandals currently causing turmoil in Slovenia.
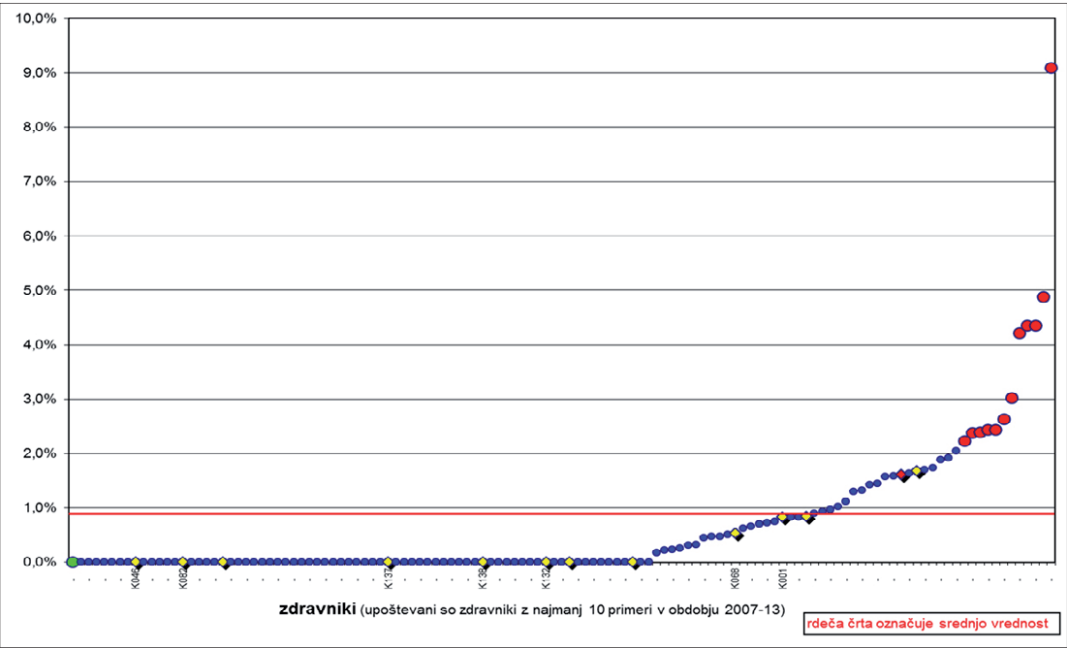
If you were unfortunate enough to have gallstones, would you want to go under the knife of a surgeon, who out of nine per cent of gallstone removal operations, inadvertently damages the bile duct, blood vessels or surrounding organs? This is one of the questions you could ask yourself after looking at the recently released chart which tracks the quality of Slovenian healthcare from the years 2012 and 2013.
This chart shows the individual doctors that operate on gallstones, represented as tiny blue, yellow and red dots, according to the proportion of damage they cause to their patients during operation. The majority of doctors do not cause any injuries, however, thirteen of them deviate negatively from the rest.
Whereas the average surgeon causes unnecessary damage in one percent of cases, the negative record holders cause around two percent of cases of reported damage. At the top of this infamous chart is a surgeon who, according to data taken from the report, injures as much as nine percent of patients.
It should be noted that the chart is also based on incomplete data. Certain hospitals do not even bother to send out the information regarding surgical complications, even though they should. At the same time, the data does not show how complicated were the cases that individual surgeons were performing. However, the poor performance of certain surgeons in itself demands an explanation. Are these surgeons not proficient in their profession? Are they perhaps in need of additional training? Are they facing any other difficulties? How to guarantee that the patients of these surgeons will not face any unnecessary health complications?
The Slovenian health system is avoiding such questions. This sad truth has been pointed out by numerous scandals that have broken out recently. Deaths of four children at the department for children cardiac surgery at the Ljubljana University Medical Centre that, according to experts, need not have happened if only they were given the correct treatment. A patient that died during resuscitation because he was given laughing gas instead of oxygen. A doctor at the neurological clinic that supposedly killed his patients with potassium because his drug usage was so poorly monitored.
These scandals are only the tip of the iceberg, indicating the neglect of the quality of patient treatment in Slovenian healthcare. They also point out deeper systematic weaknesses. The Slovenian healthcare system has no mechanisms to monitor quality in regards to the treatment of patients, and thus cannot prevent unwanted complications during treatment or even unnecessary deaths.
The issue of quality patient treatment is therefore in the hands of individual doctors or, in the best case scenario, hospital departments. If a doctor, who causes direct damage to almost one tenth of his patients during a gallstone operation, does not take this issue to heart and his superiors do not hold him accountable, nothing can prevent him from continuing to treat his patients badly. The Slovenian Ministry of Health recognizes those problems. However, they believe there is not enough political will to adjust the law on monitoring the quality of work in Slovenian healthcare.
From fractures to clinical death
It is hard to believe that one person could be subjected to so many medical errors as Ljubo has been (his name has been changed to protect his identity). A police academy graduate in his mid-thirties, who is currently a sales representative at a Slovenian IT company, has suffered from kidney disease since birth. He has been on dialysis since the age of 14, which, as he states, has never caused him any problems.
His medical troubles began over two years ago, when doctors discovered an unexplained infection in his liver. Since antibiotic treatment was not helping, a liver transplant became the only solution. However, this resulted in side effects. After the transplant at the Ljubljana Medical Centre (UKC Ljubljana), his fingers inexplicably started to die off.
According to Ljubo, doctors’ initial solution was to cut off both of his hands and legs. “I protested against it. I would not have had much of a life,” says Ljubo. The doctors were not happy with his protests. “That is the norm at UKC Ljubljana; if they do not know what to do, they will do whatever it takes to make the person stop complaining. If I had to characterize this: If someone’s eyesight is poor due to cataracts, they would prefer to just take their eyes out,” says Ljubo when he describes his experience.
Doctors were unable to explain why his fingers were dying off. In addition, they did not ask any foreign specialists for advice. They presumed it was due to excessive calcium in his blood, so they started lowering it artificially.
This form of therapy had unforeseen consequences. At the beginning of this year, Ljubo started getting cramps during regular dialysis. For dialysis patients, these are quite mild and considered completely normal, as the body loses sodium during the procedure. As Ljubo says, one can get rid of cramps by extending or putting weight on the affected limb. But in his case, even though he was lying in bed, the cramps fractured his pelvis, hip, femur, both shoulder blades, as well as an arm and a leg. The reason? A severe lack of calcium in his bones.
His fingers stopped dying off shortly after the transplant, but doctors continued lowering his calcium levels, or rather stopped replacing the calcium he lost during dialysis. “They simply forgot,” says Ljubo.
Immediately after the fractures, they began giving him calcium again. But the consequences of that mistake were grave. He was confined to a wheelchair for three months and now has to use crutches. The metal plates, used to adjust the bones in his body, are putting pressure on his nerves, which makes his whole body ache. Today, Ljubo is not sure if he will ever be able to walk normally again.
That is not the only medical mistreatment that Ljubo has sustained. As he explains, another case was when he was given a vascular proliferation medicine immediately after the liver transplant. Doctors thought it would stop his fingers from dying off. But the medicine that is supposed to be administered to the patient over the span of eight hours, was put into Ljubo’s vein in just a few seconds. The nurse made a mistake. “I almost died right then and there. Luckily, I did not bleed out. They already called the resuscitation team, but fortunately, it was not necessary.”
Things got worse during his coronary angiography. During this procedure, a probe is inserted into the artery in order to take pictures of the interior walls of the blood vessels. The robotic arm, which was supposed to stitch the opening in Ljubo’s artery, stitched up the wrong place. “After two hours, I started complaining about pain, I got pale and my blood pressure dropped from 170 to a 100 in a matter of minutes. After a few litres of lost blood, I was already in the netherworld.” Luckily, his mother came to visit him at that time and notified the doctors after noticing his condition. Through resuscitation and a quick transfusion, they managed to save Ljubo, who was already clinically dead.
In addition, instead of the three toes that were dying off, the doctors almost cut off his healthy arm. They did not remove his injured toes until October of last year. After they took him to the operating room, Ljubo noticed that there were an unusual number of people there. “I know how things work in the operating room. If there are more than five or six people, it is a complicated procedure. There were seven people present there. They had already put a mask on my face, but I noticed that my leg was still covered up when they started disinfecting my arm. Before I fell asleep, I asked them why my leg is still covered and why there are so many people present for a simple toe removal. That was when they told me that they want to cut off my arm. Luckily, I was able to tell them that I was there only for the toes.”
How is Ljubo rationalizing all these medical errors? He thinks the fault lies within the system itself and not within the individual doctors. The first problem is the vast hierarchical system. Only a handful of head doctors make all the decisions, while the others do not have a say. Moreover, doctors do not talk to their patients. “Patients have no idea what is going on and cannot decide on anything. Even if a patient knows something about their condition and could help, doctors simply disregard them.”
They also have problems with treating numerous conditions at once. “If you hurt your arm, they will treat it. But when there is more than just one condition, or if it is a serious disease, they do not know how to coordinate among themselves. I will give it to you straight: The UKC Ljubljana has three different computer systems, which are not interconnected. A doctor cannot know what is wrong with the patient if the report is in the other system!”
Head doctors amongst the worst
In 2012, in order to prevent such medical errors, the now retired professor Dr. Marjan Pajntar began systematically gathering certain information that would allow him to discover exactly which doctors, individual departments and hospitals perform better at treating patients, and which perform worse. He developed several quality indicators. One of them is the already mentioned indicator on the proportion of gallstone operations with unnecessary injury to the patient. The indicators also follow the number of bleedings and required transfusions in certain operations, as well as the number of post-operative complications, as well as those which take place during labour and some of the other unpleasant consequences of treatment.
Pajntar emphasises that the intention of monitoring errors during treatment was not to punish doctors, but mainly to improve patient treatment. With these indicators, individual hospitals, departments and doctors could determine the areas where they excel and those that needed improvement. High performing doctors could share their practices with others, while doctors who lacked necessary skills could have access to additional training. Pajntar describes a case of a perinatologist, a doctor working in obstetrics, who read the indicators and realized that she was one of the worst-performing perinatologists in the country. “Is that how bad I am?” she asked Pajntar, who then replied, “Yes, you should work on your skills.” According to Pajntar, she is now one of the best perinatologists in Slovenia.
In Slovenia, these indicators are most closely followed by obstetricians, which is Pajntar’s profession as well. For example, the indicator for the number of cerclages, a procedure where the cervix of a pregnant woman is sewn shut to prevent abortion, helped them to discover the reasons behind the above-average number of abortions and complications during pregnancy in one of the maternity hospitals. Due to the risk of premature birth, cervical cerclage is only necessary for around one to two percent of pregnant women. However, two Slovenian hospitals performed this procedure on one in ten pregnant women. Since these invasive procedures were done unnecessarily, one of the two hospitals recorded a higher number of infections and complications in pregnant women and therefore also abortions. After seeing the numbers, Pajntar tells us, they changed their practices and things improved.
Ignoring the monitoring of quality may also cause unnecessary patient deaths. Pajntar describes a case that he witnessed as a court expert. “A pregnant woman, who was bleeding, was given only glucose instead of blood. Her heart was pumping air,” and the pregnant woman died from the consequences. But the death of a woman can not be blamed on the doctor, who gave the pregnant woman glucose. The problem is within the system, emphasizes Pajntar.
In the past, maternity hospitals had a doctrine, which stated that patients should not be given too much blood, because it increases blood pressure and consequently a blood vessel in the brain could burst. “This doctrine is applicable for someone who is over 80 years old. Pregnant women are between 25 and 30 years old, and blood has to be replenished very quickly,” explains Pajntar. Therefore, the treatment doctrine should be changed. Pajntar presented this case at a perinatology conference, which was attended by representatives of all maternal hospitals, except for one. It was in that hospital that the next patient died because she received glucose instead of blood. “But they got away with it, because they settled the case out of court and paid off the husband,” says Pajntar.
Despite the positive outcome of his work, Pajntar has faced major difficulties while gathering information on the quality of work of doctors. “Someone told me I just might get away with it if I only publish information about the doctors who are the worst at their jobs. But if I publish which doctors are the best, I am done for. And that is exactly what happened. Why? Because usually the head doctors are not among the best, and that is why they do whatever they can to destroy the system,” says Pajntar.
Hiding information
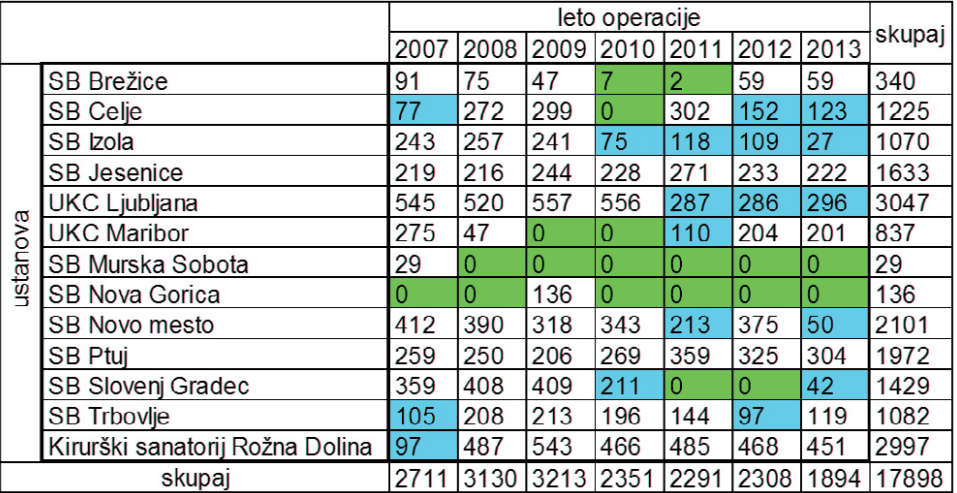
The first difficulty Pajntar faced was hospitals being uncooperative when it came to sending information about complications during individual medical procedures. Since 2010, hospitals are now obliged to send out information about individual procedures on the basis of a general agreement, which is a special contract between the Ministry of Health, the Health Fund and the medical institutions for financing the latter. The results of the data analysis are then included in annual reports on the quality of healthcare. However, despite their obligations to do so, certain hospitals still do not provide the necessary information.
Let’s take a look at a case concerning a complication during a routine gallstone removal operation. The hospitals in Murska Sobota and Nova Gorica have not transmitted any information at all in the past years. Pajntar estimates that five other hospitals are sending incomplete information. Only six general hospitals transmitted complete data for 2012 and 2013, so information is available only for the last two years. Only two hospitals, the one in Ptuj and the one in Jesenice, have transmitted complete information since 2010.
Hospitals with poor performance are usually the ones that are refusing to transmit data. An expert on this matter, who wished to remain anonymous due to the fear of backlash, describes the case of the neurological clinic at the Ljubljana Clinical Centre. The hospital was one of the worst in this field according to the data, so they simply stopped sending information about their work. Pajntar noticed the same pattern regarding the inadequate performance of the clinic. According to research, the mortality rate in three of the hospitals, admitting patients suffering a brain stroke, is around eight percent. In Ljubljana, it was 35 percent.
The problems within clinic first became public after the infamous Radan case, when the Ministry introduced professional supervision at the clinic. The supervision revealed that in Dr. Radan’s department, medicine consumption of individual patients was not accurately reported and that doctors ignored warnings from nurses. They were also not given suitable training and did not practice proper hygiene, which increased the risk of nosocomial infections.
The hospitals that do not transmit information despite their obligation to do so, are not being sanctioned. The Slovenian Health Insurance Institute (ZZZS) could interfere. They could cut part of the operational funds of hospitals if they fail to keep and transmit information about their procedures. But the Institute is not doing that, because the regulations and financial agreements do not provide any penalties for such conduct, explains Damjan Kos, the spokesperson for ZZZS. However, he does agree that such financial penalties would force hospitals to transmit information. “In our experience, punishment is the only thing that works,” says Kos.
The second problem is funding. The Institute of Biomedical Informatics at the Ljubljana Faculty of Medicine, which is led by Dr Brane Leskosek, analyses data on the quality of work of doctors and hospitals. Since 2013, they have not received any money for their operation from the Medical Association. They would need from 50,000 to 100,000 euros per year to analyse and prepare quality indicators.
The Vice President of the Medical Chamber, Dr Valentina Sojarja, explains that despite numerous initiatives given to the Ministry of Health and their promises, the issue of quality has been at a dead end in recent years. This goes both for changes in organisation and funding. The Medical Chamber of Slovenia decided to stop financing the project due to the lack of orderliness and clarity on the systematic level. The current system can not reflect the actual situation and is, among other things, in need of a comprehensive substantive and infrastructural reform, says Sojarja. The Medical Chamber states that they are ready to develop the project further, but only if they can guarantee a more wholesome approach to quality in healthcare.
The consequence of the lack of funds is outdated data. As mentioned, it was only this year that the Ministry of Health published the report on the quality of healthcare for the years 2012 and 2013. Due to a lack of funds, publication of more recent data is not in sight.
The third problem is a lack of appropriate measures being implemented on the basis of discovered deficiencies, which is shown by quality indicators.
Certain clinics, like the gynaecological clinic at the Maribor University Clinical Centre and the department for thoracic surgery in Ljubljana, asked Pajntar for recent data in order to assess which areas still need improvement. Meanwhile, other departments simply ignore the results. Some doubt the methodology of gathering and analysing data, explains Pajntar. For example, they claim that their average cases are more complicated, which is why their patients face medical complications more often.
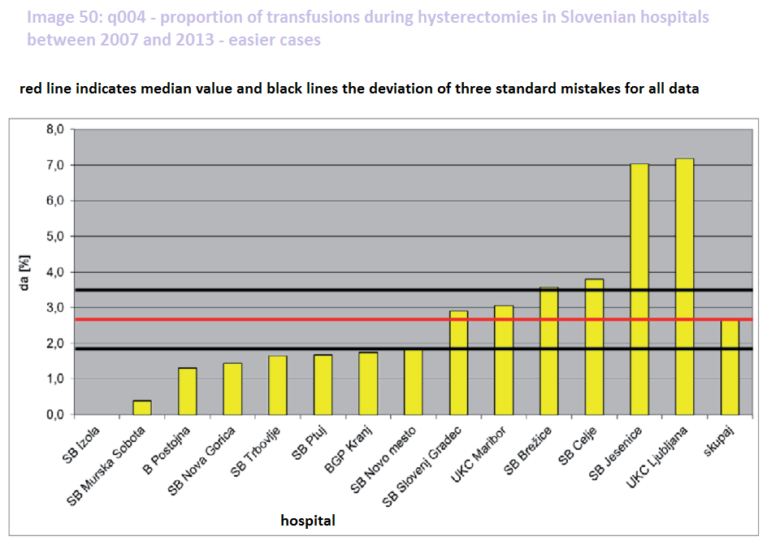
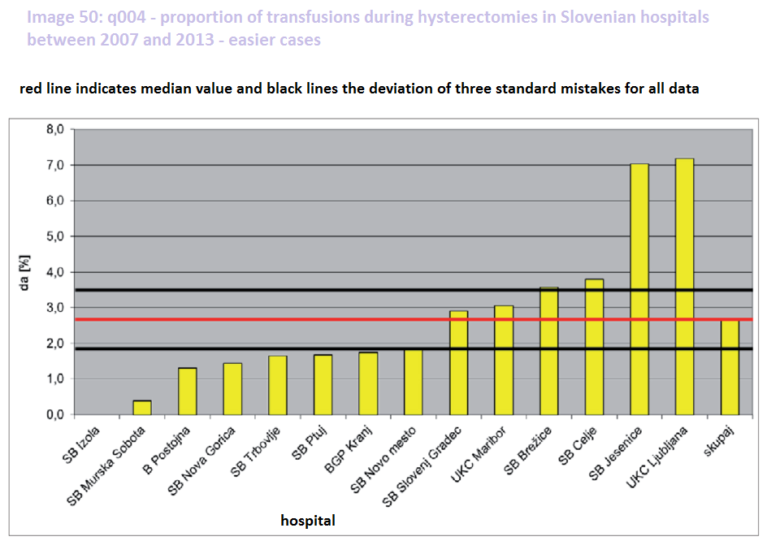
In return, Pajntar points out his analysis. Studying hysterectomies (uterus removal operations), he analysed the number of transfusions in both simple and complicated cases. He found that the difficulty of the operation does not have an impact on the success rate of the clinic, since the clinics that need to give more transfusions in difficult cases due to high loss of blood, also tend to perform poorly in simpler cases. The worst performing is UKC Ljubljana, where they need to give a transfusion to 16 per cent of the patients in difficult cases and to seven per cent of the patients in simpler cases. The average for all hospitals is only six percent for difficult operations and three per cent for easier cases.
Hand in uterus without permission
UKC Ljubljana, which is supposed to be the most prestigious healthcare institution in Slovenia, has a bad record in the field of obstetrics, according to the health indicator for children after childbirth. The health indicator measures how many newborns score from one to six on the special ten-stage Apgar score. In simpler terms: The higher the Apgar score of a newborn, the healthier the baby is right after childbirth. Score seven or up represents the normal state of a newborn, whereas lower scores indicate health problems. In UKC Ljubljana, almost 1.6 per cent of newborns were born with a score six or lower, while the average score in maternity hospitals is two times lower. UKC Maribor, which ranks second, currently has a score lower than one.
Meta (her name has been changed to preserve anonymity) had a bad experience during labour at UKC Ljubljana. In the spring of 2008, when her baby was due, she still had not gone into labour. She had a check-up at the gynaecological clinic, where the gynaecologist checked her condition and gave her another appointment in two days time. She also advised her to walk a lot in order to induce labour.
Before her next appointment, Meta went for a long walk. The check-up showed an accelerated heartbeat of the foetus. Instead of a normal 120 to 160 beats per minute, the heart was beating at 170 beats per minute. The gynaecologist explained that the long walk could have been the reason for the accelerated heartbeat, but that she still needed to send Meta for an examination at the maternity hospital at UKC Ljubljana.
Upon Meta’s arrival, a male doctor and another younger doctor or resident received her. “What followed afterwards, was something I could not have imagined in my worst nightmares. After the doctor touched the cervix, he pushed his hand deeper and started scratching. I was overwhelmed by the unbearable pain and in that moment, I knew exactly how a rape victim must feel. I was shouting out in pain and horror, because someone just violated my body without asking or explaining anything. The younger doctor was stared shockingly, first at the doctor then at me and then back at the doctor, who only commented that I am ‘too sensitive’ and that I should wait in the waiting room. I almost ran out of the clinic in tears and then found refuge in the toilet, because I could not bear sitting among other people in my state. There, I started feeling a pain in my stomach and noticed blood and mucus on my underwear,” describes Meta. Without asking her, the doctor performed a membrane stripping to induce labour.
After a sleepless night at the hospital due to a horrible pain in her stomach, Meta gave birth in the morning. Because of stress and previous violation of her body, it did not go smoothly. The baby descended down the birth canal, but Meta was unable to do the final push, in order to bring the baby into the world. The child’s heart rate fell to a dangerously low level of 60 beats per minute. “First, a female doctor ran in and after her the male doctor, who dismissively remarked that ‘I would have pushed, had I wanted to’. The room fell into a panic; my legs were suddenly strapped in and the doctor stepped between my legs with some instrument. I knew that what followed was the vacuum extraction. They cut my perineum (judging by the stitches probably more than just that) and out came our boy,” recalls Meta. Childbirth with the help of vacuum extraction is very risky. In worst case scenario, the baby’s skull can be broken and it can potentially cause internal bleeding.
What does UKC Ljubljana have to say to the critics? Have they found out why are they among the worst Slovenian hospitals according to some indicators? We posed these questions to Dominika Oroszy, the Assistant Technical Director for Quality at UKC Ljubljana. The latest report on quality indicators was released only a few weeks before the interview, so UKC Ljubljana has not yet studied the results. However, Dominika Oroszy assured us that they intend to do that in the future.
Pajntar’s data taken from the annual reports on the quality of healthcare is otherwise being criticised by UKC Ljubljana. Dominika Oroszy thinks it is too subjective, because of the differences in hospital reporting. The doctors themselves have to report the complications during treatment of their patients, which supposedly makes it unreliable. However, Oroszy admits that UKC Ljubljana never introduced any sanctions for those doctors and departments that failed to file in the reports, even though they are contractually obliged to do so. “The culture of hospital reporting is bad everywhere and so far there has been no culture of understanding that this indicator is a means for improvement. There is also no transparency,” says Oroszy.
UKC Ljubljana has been developing its own programme for quality monitoring since 2013. At that time, they joined an international initiative, which includes hospitals in Switzerland, Austria and Germany. The information on treatment of their own patients is being collected in so called “Groups of comparable cases”, on the basis of which hospitals receive money for patient treatment from the Health Fund. The bases have information for each individual case and include the diagnosis of the patient and the information on whether they have died. At UKC Ljubljana, they then compare the death rate with the rates of the international hospital initiative.
For example, with the help of this analysis, they already discovered a high mortality rate because of sepsis i.e. bacterial blood infection. According to the data taken from UKC, the reference hospitals aim to have a 17.7 percent mortality rate in cases of sepsis. At UKC Ljubljana, as much as 28 percent of patients died due to this complication last year. Because of this, they sent their staff to additional training in this area and prepared a programme for early detection of sepsis. According to Oroszy, when it comes to sepsis, early detection is key, which means timely antibiotic therapy. At the same time, they improved their hygiene practices and as Oroszy states, the “responsiveness of their staff on hand disinfection is significantly better than it was a few years ago”.
However, indicators from UKC Ljubljana do not measure the success of individual doctors. As Oroszy explains, these are only just being prepared. First, they need to define what they will measure, such as complications during medical procedures, number of treatments or other factors. By June, they will propose a collection of five to ten indicators for individual doctors, assures Oroszy.
UKC Ljubljana would also like the Ministry of Health to play a bigger role in quality assurance. They wish for a joint strategy and measures for improving the quality of Slovenian healthcare. “In order to determine at the national level where we perform better or worse, and what should be done first. We would also like a suitable IT support for collecting the indicators. Because, honestly, many indicators are being collected manually and then entered into an Excel table,” says Oroszy.
No political will for improved healthcare
The State Secretary at the Ministry of Health, Sandra Tušar, has experience with quality assurance, judging by her career path so far. Before joining the Ministry, the general surgeon specialist used to be the Director of the hospital in Jesenice and a member of the hospital’s quality board. The hospital in Jesenice used to have a problem with a high number of transfusions during labour. But, according to the observation of Dr Marjan Pajntar, the hospital managed to turn things around in the past years. What was wrong and how did they manage to change the trend?
“Our surgeons were old school and they only gave blood to a patient as some kind of a treat and not when it was proven that a treatment is better with transfusion,” explains Tušar. Foreign blood is a foreign body, which makes blood transfusion risky on its own. They managed to lower blood consumption by improving operating techniques and changing clinical guidelines on when a woman actually needs a blood transfusion.
Tušar says that she would like to introduce quality indicators in all Slovenian clinics. But, which indicators? Those developed by Marjan Pajntar? Or the indicators introduced by UKC Ljubljana? Maybe something else entirely? According to the State Secretary, Pajntar’s indicators pretty much revealed actual conditions at individual hospitals and their departments. However, she also believes they were less reliable for evaluating individual doctors. Including the intention to reform indicators, the Ministry founded the Board for quality and safety in healthcare. They do not yet know what kind of indicators they will prepare specifically. However, they will add indicators that show the attitude of the hospital towards the patient. One such indicator will be how long a patient has to wait for his release papers after leaving the hospital.
Defining the indicators is not the only problem the Ministry faces. Just like Pajntar, the Ministry also has problems with certain hospitals, which do not transmit all the data. “Certain providers actually told us that we cannot in any way force them to report to us,” says Tušar. For this year, and no later than the beginning of 2017, she announced the adoption of laws and secondary acts, which will clearly define hospital obligations, as well as sanctions for those who do not transmit the necessary information.

But not even this legislation can solve the biggest issue. What is the point of gathering data, when hospitals, departments and individual doctors are not prepared to improve their work after receiving bad results?
“I absolutely agree that monitoring individual doctors that show a negative deviation is not systematically introduced,” says Tušar. The improvement of their work depends on their leader and then on the hospital director. If they do not intervene, such doctors could continue to pose a threat to their patient. This is where the Ministry or another independent institution should step in, measure the results of quality and regularly control what improvements the hospitals introduced in the areas where they were lacking.
Up until three years ago, the Ministry controlled hospital functionality up to a certain degree, explains Sandra Tušar. Each year, after the publication of quality indicators, the ministry made a special demand for hospitals to present measures for improving the areas in which they were not performing well. But the system broke, mostly because of the quick succession of Ministers. The Department for Quality at the Ministry also suffered from alack of funds. The funding has now been replenished, according to Tušar. Now, the Ministry will demand that hospitals report on measures for monitoring and improving their quality of work again.
However, the key component for providing quality patient treatment, Ministry verification of whether or not the hospitals are actually implementing the measures for improving the quality of patient treatment and whether or not these measures are actually proving themselves to be effective, will not be in place for a long time, admits Tušar. The end goal would be the establishment of an independent agency for quality control in healthcare, which would collect and analyse data, report on the results of individual health facilities and then advise the latter, as well as monitor the measures for quality improvement. “But do not ask me when this will happen.” Why not? “I do not believe there is the political will at this moment to establish such an agency. The reason for this is probably lack of money. There is no money to hire ten people that could work in this area for a whole year,” says Tušar. Out of all the billions of euros decanting through Slovenian healthcare.
We need norms
“In Slovenia, the quality of patient treatment means nothing. We are still in the past, when it only mattered how much you did. If you made 5,000 handles and half of those were bad, you reported that you made 5000 handles. Nothing else mattered,” Dr Marjan Pajntar, a pioneer in collecting data on the quality of work of doctors in Slovenia, assesses the attitude towards quality in healthcare.
Implementing norms in the area of quality in healthcare could also contribute towards changing the overall culture. Current norms mostly tell the hospitals only how much time a doctor should spend on one patient. However, there is nothing written on what the outcome of treatment should be, highlights Sandra Tušar from the Ministry of Health. Quality norms should therefore be introduced especially in the area of payment for medical services. The health fund pays healthcare providers, such as hospitals and clinics, for their services based only on the number of check-ups, operations and diagnoses. “Sooner or later we will have to start paying not only for the quantity of work, but the quality as well.” However, there are currently no laws on what a quality medical assessment should look like. “There are no clinical guidelines, on the basis of which the payer for healthcare could tell the healthcare facilities that they did not abide by the clinical guidelines in their treatment process and therefore pay them less for their services,” says Tušar.
In future, such a system will most likely be implemented, but systems cannot be changed overnight, emphasises Sandra Tušar,. The Ministry is preparing amendments to the Health Care and the Health Insurance Bill, which will lay the groundwork for such a system. As Tušar says, the moment that your salary depends on the quality of your work, you adapt to it sooner or later.
Nastanek tega članka ste omogočili bralci z donacijami. Podpri Pod črto
Deli zgodbo 0 komentarjev


0 komentarjev